In 1990, I established the Gethsemane Community in inner-Sydney Marrickville for homeless women and men with mental ill-health and intellectual disability. It was an alternative to the transient model that had transpired from the 1983 Richmond report into mental health in NSW. The report recommended “deinstitutionalisation”, but many of the “deinstitutionalised” ended up on the street and/or relocating from one “boarding” house to another. I found it was much better to keep people in a secure “family-like” environment. The different emphasis allowed me to improve their living skills with an aim of independence.
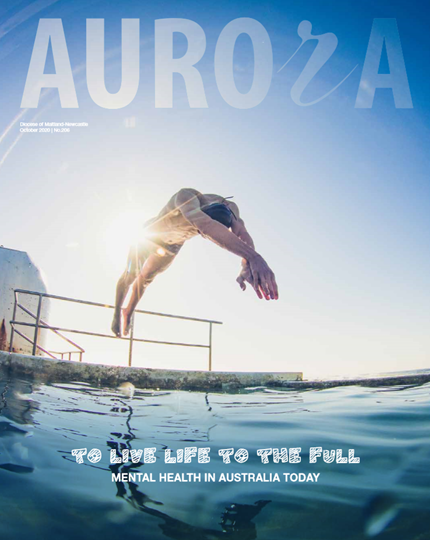
The connection between homelessness and mental ill-health and other types of disadvantage is unavoidable. It is reported that 75 per cent of homeless people have mental illness. This mental ill-health is often associated with other conditions, such as intellectual disability or addiction, but in most cases it is schizophrenia-affected disorders along with depression and anxiety. The complexity makes it difficult for them to access appropriate but diminishing mental health services.
A decade on from the Richmond report, the National Inquiry into the Human Rights of People with Mental Illness released its findings. Commissioner Brian Burdekin supported the views of those of us at the coalface. People with mental ill-health newly on the street as a result of the Richmond report lacked proper support. The money that had previously gone to institutions never followed them into the community.
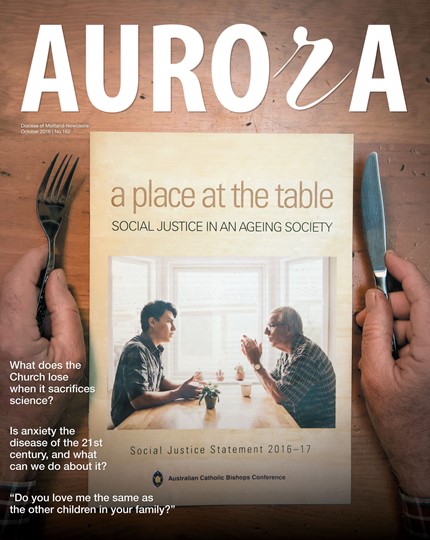
Today, the Australian Catholic Bishops Conference’s Social Justice Statement 2020-21 correctly refers to the “missing middle” – the severe lack of specialist community mental health services and after-hours care. The Social Justice Statement notes Australia spends more than $10 billion on mental healthcare each year, but we still have a disjointed and complex system of services that are difficult to navigate. Gaps between primary healthcare and acute care result in people falling through the system. Starved of funds, I have seen the community mental ill-health system atrophy before my very eyes.
Homelessness can cause or exacerbate mental ill-health. The Down and Out in Sydney study of 1998 reported many homeless people had trauma. The prevalence of schizophrenia in the general population is 1 per cent, yet the Down and Out study found that for homeless men on the street it was 23 per cent, and for women on the street it was 46 per cent. The women you see on the street are often much more complexly ill than the men.
Housing-first is the answer to long-term homelessness and rough sleepers. Finland ended street homelessness in 10 years. Its population, 5.5 million, is similar to Ireland’s (almost five million). Both countries addressed street homeless about the same time, 2007-08. Ireland built more shelters. Finland adopted the housing-first approach, converting all its shelters into permanent residences, and building other accommodation. Working at the problem systematically it assessed the affected people and put out tenders to NGOs for support services. Finland now has one shelter in the entire country, with 50 beds that are not full. The official figure of Ireland's homeless still wavers around 10,000, but experts say the actual number is far higher.
Secure housing is the first step to any kind of solution to mental ill-health, addiction, and the dual diagnosis of both. If someone has somewhere secure to live, the people who can help them can easily find them. Secure housing also alleviates trauma.
Successful programs, and studies, show the housing-first approach is far cheaper than the prevalent merry-go-round. With crisis-only psychiatric services and patients referred to their GPs, the homeless are just cycling through the system. It’s an expensive revolving-door approach. And it goes on. Consider the cost of city teams looking for the homeless, state and federal teams “working” for the homeless, ambulances, health services, police, the legal system, jails, and hospitals.
Gethsemane offers secure housing, with tenancy rights, support, and assistance to learn living skills. Residents sleep without anxiety or depression in their own big rooms.
It is important that faith communities are aware of the mental ill-health crisis. This is where the bishops’ statement and the associated resource 'Do Not be Afraid' Mental Illness and Outreach Guidelines for Parishes can help.
Saint Mary MacKillop worked with homeless suffering ill-health. A housing-first approach today would provide a cost-effective solution to this problem while applying her values of love, justice, compassion, and dignity.
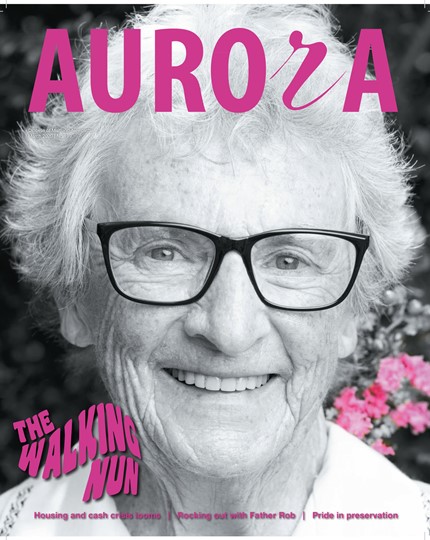
Sr Myree Harris rsj OAM is the founder of the Gethsemane Community – a home for the homeless – www.gethsemanecommunity.org.au. She was part of the working group that prepared the 'Do Not be Afraid' Mental Illness and Outreach Guidelines for Parishes.