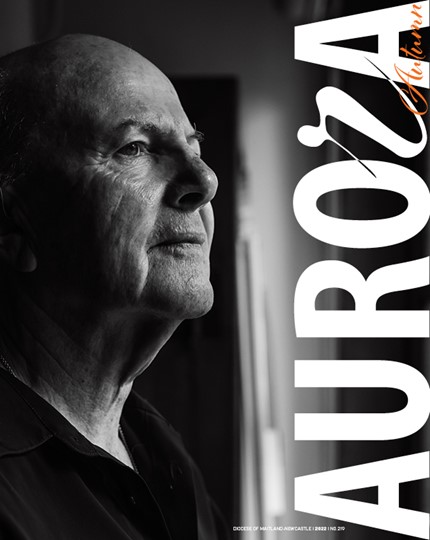
A diagnosis of terminal cancer or other life-limiting illness is a distressing experience for anyone, but more recent advances in Palliative and Supportive Care are putting patients back into the driver’s seat when it comes to deciding how their treatment will unfold and how they and their family will experience the journey ahead of them.
Although a relatively new area of medical specialisation, Palliative Medicine has developed in recent decades into a sophisticated, patient-centred, multidisciplinary approach to care.
It is this attention to the whole person that sets it apart from other medical specialities, says Associate Professor Natasha Michael, Director of Palliative Medicine at Cabrini Health in Melbourne.
“The World Health Organisation definition of Palliative Care is very explicit, that it is about providing holistic care, where you pay attention to the physical, the psychosocial and the spiritual dimensions of support and care to patients and families living with a lifelimiting illness,” she says.
“It also talks about early integration, so that you see people early on in their disease trajectory, when they’ve just been diagnosed with such a condition, and you provide care through the illness continuum, and right through to the bereavement period for the family. And that care is provided by a multidisciplinary team.”
Dr Maria Cigolini, Clinical Director of Palliative Medicine at Royal Prince Alfred Hospital, Sydney, says many people’s fears of death and dying stem from bad experiences with the death of a loved one in the past.
“In the past, people didn’t really talk about dying and there were a variety of problems that would occur around death which would go unmanaged,” she says.
Dr Cigolini says recent decades have seen a rapid growth in cancer medicine, as well as treatment of other chronic diseases, such as in heart and renal disease, meaning that people often live longer with progressive disease and develop more symptoms.
“Our role is to try to keep people symptomatically well and controlled to get on with their life, as well as being able to get through their treatments to prolong their lives,” she says.
“When the disease becomes refractory to treatment, then our role is to assist them in planning in advance how they want to be managed when curing the disease is no longer a priority.
“This would include considering such things as place of death, how they want things to be for them, as well as supporting them in the community to either achieve a death at home or to be kept at home as long as possible through community palliative nurses and doctors in cooperation with the GP and specialists. And an important role is also to support relatives, friends and carers in their role to be able to live this part of their lives the best they can until death ensues.”
Dr Cigolini says that one of the most important aspects of good palliative care is that it can return a measure of control to a patient who might feel their life had spiralled out of control upon diagnosis.
“With all the resources we now have and the human experience in dedicated social workers, psychologists, chaplains, therapists and wonderful nurses, this time of dying becomes a very human and whole experience,” she says.
“I feel we can really say that it is definitely possible to have a good death. It is possible and it is happening.”