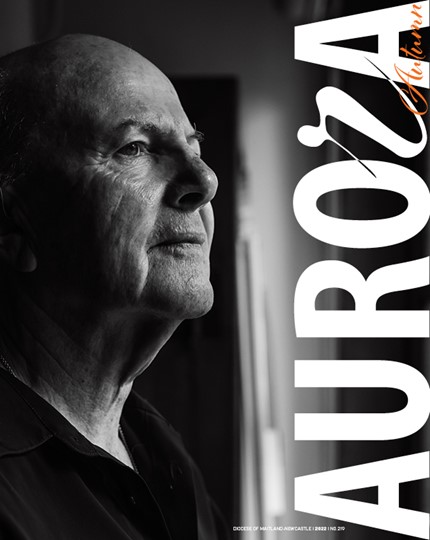
It was said that Father Giuseppe Berardelli refused a ventilator, insisting that it be allocated to someone younger. Or, as the papers put it, Fr Berardelli ‘donated’ his ventilator to someone younger.
Fr Berardelli was a well-loved priest. Perhaps that is why the story began to circulate. (The hospital - rightly - would not comment.)
But a close friend of the priest explained what had really happened. By the time Fr Berardelli got to hospital he was already too sick to be helped by the ventilator. He had other things wrong with his health as a result of which he simply could not tolerate this form of treatment.
The story – mistaken but inspiring - indirectly raises an important question in medical ethics. How should medical resources, for examples ventilators or beds in intensive care be allocated if there are not have enough of them for all those who need them?
If sick people find themselves, through no fault of their own, competitors for the same resource, what policies should inform the decisions made by those with the responsibility for deciding whose treatment should take priority?
Of course, we all hope that it won’t come to this in Australia: that’s the point of the current severe measures which are intended to slow down the pace of the spread of this virus. But it would be negligent of hospitals to fail to prepare for the worst whilst hoping for the best. And it might be head-in-the-sand for the rest of us to ignore the issue.
A good way to begin to think about this question is to identify ways of allocating resources which would certainly be unjust. What factors ought to be treated as morally irrelevant the distribution of resources? Let us get them out of the way first (because some of them have been ‘doing the rounds’ recently.
An obvious one is a person’s skin colour: other things being equal, there is no defensible reason why a black-skinned person should be offered treatment ahead of a white-skinned person. That would be unjust.
Another obviously irrelevant factor is a person’s capacity to pay for expensive treatment: other things being equal, there is no defensible reason why a relatively-affluent person should be offered treatment ahead of a relatively-poor person. That would be unjust.
A third, not so obvious perhaps, is a person’s age: other things being equal, there is no defensible reason why a younger person should be offered treatment ahead of an older person. That would be unjust.
Of course, age is sometimes an indication (or ‘proxy’) of other things (such as extreme frailty) which may be relevant to therapeutic decision-making. In and of itself, however, age ought to be irrelevant.
What factors ought to be considered relevant? What are the requirements of ‘justice in the allocation of healthcare resources’?
Obviously, the need for treatment is where we should start. So, by extension, medical needs should be addressed in order of importance and preference given to the patient in greatest need.
That is the right starting point. We can go further and spell out some applications of this idea.
If choices become unavoidable, between two patients, then it would be reasonable (that is, just, defensible) to give preference, other things being equal:
- to the patient whose need is more urgent,
- to the patient who is more likely to benefit therapeutically from the available treatment,
- to the patient who is likely to gain the greater or longer therapeutic benefit from the treatment,
- to the patient who is likely to suffer the lesser burden from the treatment,
- to the patient who is likely to suffer the greater harm without the treatment,
- to the patient who is less at risk of various ill-effects from the treatment,
- to the patient who is likely to gain the same therapeutic benefit from less of the treatment,
- to the patient who is likely to need the treatment for a shorter time or less frequently,
- to the patient who has fewer or no alternative avenues of satisfying the need, or
- to the patient who is more likely to infect others if untreated.
These might be called ‘priority criteria’. They build on the practice of triaging patients according to need. That’s a practice which is familiar to anyone who has had to wait for treatment in an emergency ward. There it is not ‘first come, first served’ (or at least it should not be) but ‘give priority to the person whose need is most urgent’.
Some of these priority criteria come directly from a Christian commitment to the poor and vulnerable: the homeless, those suffering from disabilities or addictions or compromised mental health, those living in remote communities, etc.
Most of them are extensions of the normal practice of Hippocratic medicine. On the one hand, patients have the moral right to refuse any treatment. On the other, good doctors do not provide (nor even recommend) treatments they think would be therapeutically ineffective. In addition, good doctors are always sensitive, in their recommendations, to the possibility that a treatment will impose burdens - on the patient, on the family, on the wider society.
Archbishop Anthony Fisher, the chief author of the book published twenty years ago from which these priority principles are taken, suggests that a good way to test them goes something like this: Would I think that these principles of allocation were fair if I (or someone I loved) were in healthcare need, particularly if I were one of those likely to be excluded from treatment or were among the weakest in the community?
The story about Father Giuseppe Berardelli ‘donating’ his ventilator to a younger person, though fictional, is inspiring. We shall need its spirit of generosity and fellow-feeling in the coming hard days. But we shall also need that Christian, and Hippocratic, sense of justice that good doctors show as they fulfil their professional responsibilities in often-trying circumstances.