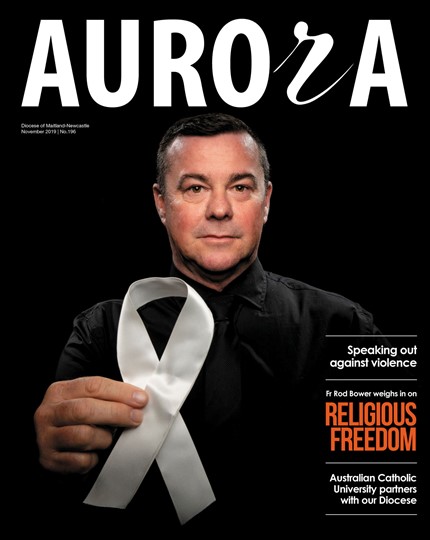
In September, Queensland became the fifth Australian state to adopt VAD. NSW looks set to follow soon. The Independent Member for Sydney, Alex Greenwich, has introduced his bill – co-sponsored by 12 Labor MPs – and it is being debated in the Lower House. The new Premier, Dominic Perrottet, has assured Liberal MPs they will have a conscience vote and an Upper House committee will examine the bill in detail.
Generally, this is reported as a victory for the left, part of the gradual progressive shift that inevitably occurs over time. But even if we are to accept that this left versus right framing of VAD was accurate in the past, it doesn’t hold in 2021. The critical factor that’s changed over the past decade is medical science, primarily in the field of palliative care.
You’ve probably never heard of intrathecal care. It’s a new drug-delivery method palliative care specialists use in which a catheter is inserted near the spinal cord, similar to an epidural. It enables pain relief while allowing mobility and lucidity. Likewise, you may not know about nerve blocking, where pain specialists inject a numbing substance into a group of nerves.
These kinds of medical advances change the game on end-of-life care. When most of us think of palliative care, we picture a nurse increasing the morphine dose until a bed-bound patient slips into a barely responsive state. But palliative care specialists administering modern pain treatment doesn’t just manage psychoexistential suffering – it extends life.
So why is this relevant to the left-right debate? Because only a tiny fraction of our population has access to this modern palliative care. If you are among the privileged few who are very wealthy, live in the right area, or have great health insurance, you can get access to life-extending modern palliative treatments.
With them, you can likely make the most of almost every day that modern medicine enables you to have. You can use that time to connect meaningfully with family and friends, do the things you love, arrange your affairs, and plan your legacy.
But if you’re poor, live in the wrong area and have no health insurance, your chance of accessing modern palliative care is close to nil. If you are offered any end-of-life care – and there’s no guarantee you will be – it will look far more like the 20th-Century model than the modern possibilities.
We could fix this. The Australian Medical Association estimates it would cost about an extra $275 million a year to make quality supportive care available to all terminally ill Australians who need it. So, it’s expensive, but certainly possible. It’s a choice that a progressive government could and should make.
Instead, what we are offering the majority is death. I understand the apparent logic of this. If someone we care for – perhaps our mother, partner, or even our child – is gravely ill and suffering, it is a natural compassionate response to want to grant a peaceful release. But we must recognise that death is not the only release option available today.
Surely any progressive and compassionate government in 2021 should be pushing for the average person to get modern palliative care, long before they get access to death. If we continue along the path we’re on, you can easily project the result if we offer VAD and not modern supportive care. It will be
a society in which terminally ill rich people get to extend their lives, achieve some level of closure and peace, and then die without pain. Terminally ill poor people, on the other hand, will be increasingly pressured to shuffle off and die quickly, “with dignity”.
A person who doesn’t have a loving family around them might well feel steered towards ending their life through assisted dying. We see this in Canada, where almost one in six people said loneliness influenced their decision to die through medical assistance.
If voluntary assisted dying becomes available and normalised, governments won’t feel the pressure to expand palliative care and the support it offers.
If my friends and colleagues in parliaments voting on VAD laws don’t factor in quantum advances in palliative care, they will risk accidentally adopting a position that’s a betrayal of average citizens.
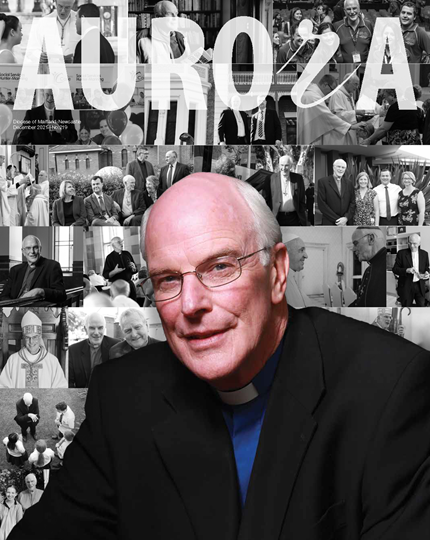
Author: John Watkins is the chair of Catholic Health Australia and former Labor deputy premier of NSW.
This edition went to print at the end of October, prior to the Lower House undertaking a conscience vote on the VAD bill.