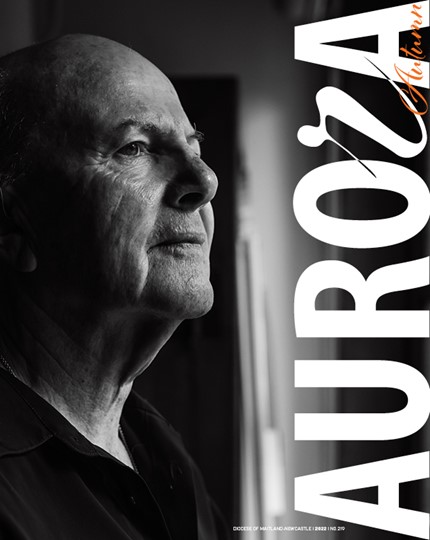
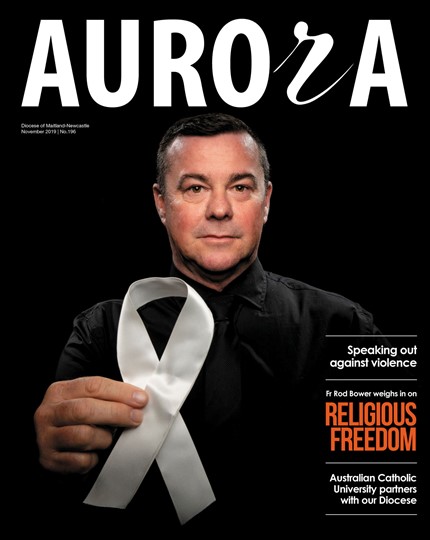
Dr Somerville, who is a Professor of Law,Professor in the Faculty of Medicine, and Founding Director of the Centre for Medicine, Ethics and Law at McGill University in Montreal, Canada, was speaking at the University of Notre Dame (Sydney), as part of a series of public lectures on ethical issues surrounding euthanasia and assisted suicide during her recent visit to Australia.
Her presentation focused on lessons to be learnt from the debate in Canada, where the Supreme Court earlier this year struck down a ban on doctor-assisted suicide for mentally competent Canadian patients with terminal illnesses.
She said one of the key arguments of pro-euthanasia advocates was that euthanasia is no different from medical treatments, such as palliative sedation, that are already widely practised.
“When used correctly as part of palliative care, palliative sedation is not euthanasia,” she said. “In palliative sedation as part of standard palliative care, physicians often allow the patient to become conscious from time to time and use the lightest possible sedation consistent with relieving suffering. As well, it’sonly used as a last resort, and not often.”
Dr Somerville said acting with an intention to kill is “different-in-kind” from allowing a natural death and that doctors are one of the groups most opposed to euthanasia.
She said that in The Netherlands, where euthanasia is legal, there is so much resistance by physicians to carrying it out that the government has had to set up “mobile euthanasia units” to visit homes and attend to euthanasia requests.
“Euthanasia is not just an incremental expansion of current ethically and legally accepted end-of-life decisions, such as refusals of life-support treatment, as pro euthanasia advocates argue,” she said.
“It seems that most politicians and many Canadians do not recognise the momentousness of a decision to legalise euthanasia. It’s not incremental change, but rather a radical and massive shift in our society’s and civilisation’s foundational values.”
Dr Somerville said another pro-euthanasia strategy to be resisted is the euphemising of euthanasia by calling it “medical treatment” and “medically-assisted death”.
“Euthanasia is not medical treatment.Defining it as such presents serious dangersto patients, the trust-based physician-patientrelationship, and medicine,” she said.
The medicalisation of assisted suicideestablishes suicide as a legitimate responseto suffering, thus endorsing suicide, DrSomerville said. Studies have shown that more honest language such as “state-sanctioned suicide” or “physicians killing their patients” reduces public support for deliberately inflicted death.
“Words matter,” she said. “Language affects emotions and intuitions, including moral intuitions, which are important to ethical decision-making.”
Drawing on the Canadian experience, Dr Somerville said the appeal to individual autonomy, to empathy and compassion,and the promotion of the idea that death is actually a benefit to someone whose life is affected by illness, were all pro-euthanasia arguments to be vigorously resisted.
She said the dangers of legalised killing to society as a whole must outweigh individual circumstances.
“Euthanasia is special (among ethical debates) because there’s nothing new about it. We’ve always gotten old, suffered, become terminally ill, been dying and somebody could have killed us, and we said ‘No, that is wrong. We don’t do that.’
“So that’s why euthanasia is so important. Because if we change that, we’re changing the very roots of our society. I think we’re changing the essence of what it means to be human if we start killing each other.”
Dr Somerville’s presentation at The University of Notre Dame was a joint initiative of the Faculties of Medicine and Law and the University’s Institute for Ethics and Society.